In a recent study published in the journal JAMA Network Open, researchers examined the clinical use of dexamethasone for hospitalized patients with coronavirus disease 2019 (COVID-19) respiratory illness and explored the heterogeneity of treatment outcomes across different subgroups.
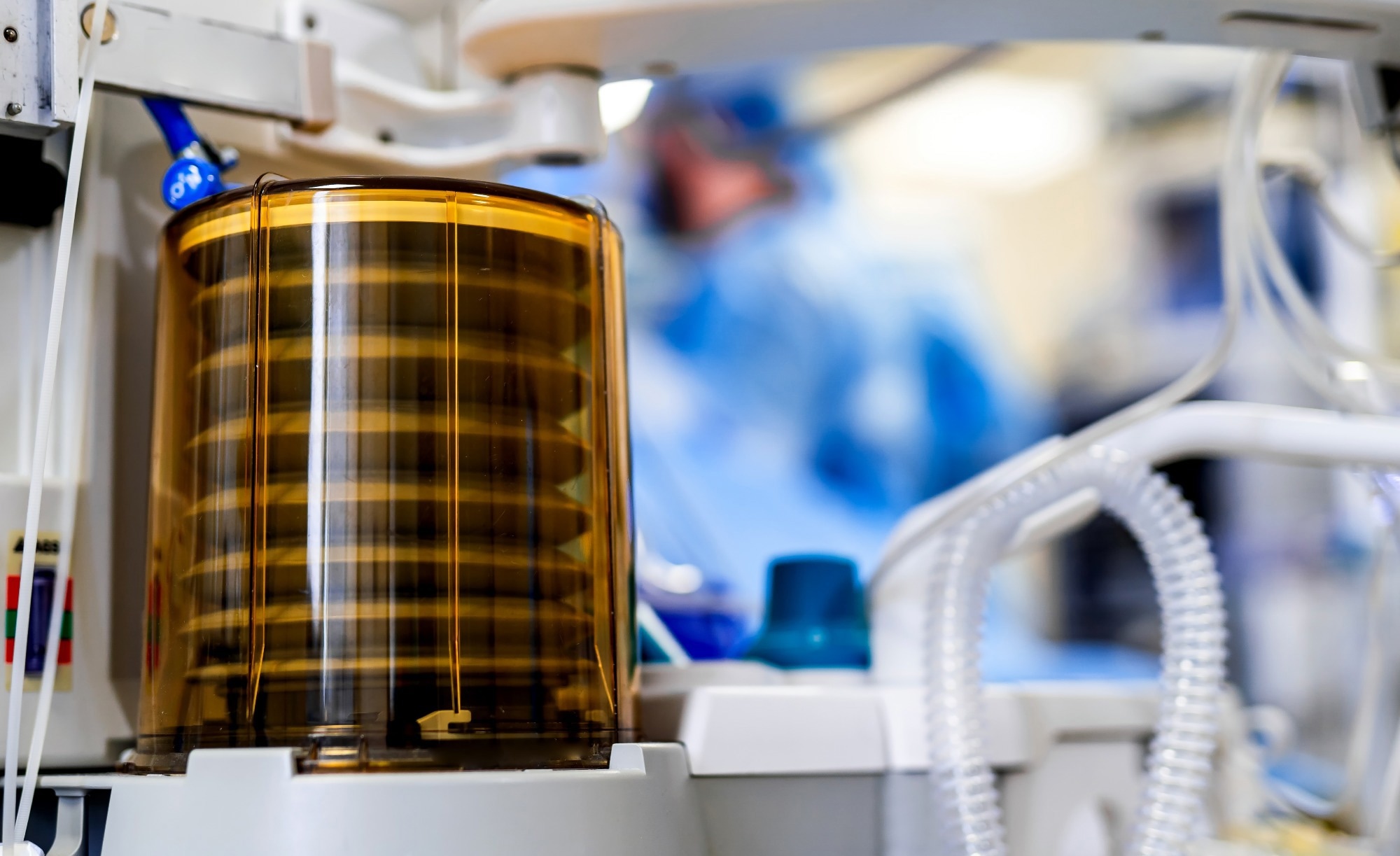 Study: Dexamethasone for Inpatients With COVID-19 in a National Cohort. Image Credit: Terelyuk / Shutterstock
Study: Dexamethasone for Inpatients With COVID-19 in a National Cohort. Image Credit: Terelyuk / Shutterstock
Background
COVID-19 has caused unprecedented morbidity and mortality across the globe. The scarcity of effective anti-severe acute respiratory syndrome coronavirus 2 (anti-SARS-CoV-2) therapeutics warrants further research to reduce the health burden of COVID-19. The National Institute of Health (NIH) has recommended systemic corticosteroid use for hospitalized COVID-19 inpatients requiring oxygen supplementation, primarily based on the findings of the Randomized Evaluation of the COVID-19 Therapy (RECOVERY) study.
However, the study did not include placebo groups and lacked a defined standard of care. Further, several categories of oxygen supplementation were combined, and the rate of death from COVID-19 was high among controls. Smaller trials examined the protective benefits of dexamethasone and systemically administered corticosteroids and reported therapeutic effects but with varying effect sizes. Moreover, an in-depth understanding of dexamethasone usage outcomes among particular subgroups of patients is lacking and requires investigation to aid in identifying patients who would benefit the most from the treatment and, thereby, increase the precision of treatment.
About the study
In the present national-level multicenter retrospective cohort study, researchers investigated whether early administration of dexamethasone among hospitalized individuals with SARS-CoV-2 infection-associated pulmonary disease in the United States (US) could improve in-hospital disease outcomes.
The propensity score-matched (PSM) study cohort included adult COVID-19 patients above 17 years of age, hospitalized for ≥2.0 days due to COVID-19-associated pulmonary disease between 1 July 2020, and 31 October 2021, at 156 United States (US) hospitals. The data were analyzed between March 2022 and February 2023. Data were obtained from the participant’s electronic medical records and compiled by the COVID-19 Healthcare and Academia Research Generation Consortium.
The study exposure was systemic (oral or intravenous) dexamethasone use within two days of hospitalization or an increase in oxygen supplementation. The primary study outcomes were any-cause mortality and hospital discharge for hospice care. Logistic regression modeling was performed to calculate the adjusted odds ratios (aORs) after adjusting for age, race, ethnicity, sex, Charlson comorbidity index (CCI) scores, remdesivir administration, diabetes, and the maximal daily flow rate for supplemental oxygen.
COVID-19 was diagnosed using the International Classification of Diseases, Tenth Revision (ICD-10) codes. Supplemental oxygen levels were categorized using a modified version of the World Health Organization (WHO) COVID-19 ordinal scale. Individuals with consecutively missing ordinal scale data and patients receiving dexamethasone prior to hospitalization were excluded from the analysis.
Results
In total, the team identified 80,699 individuals satisfying the inclusion criteria, among whom the median age was 64 years, 47% (n=37,606) were female, 16% (n=13,230) were Blacks, 61% (n=49,222) were Whites, 25% (n=20,340) were Hispanics, and 23% (n=18,247) were non-Hispanics. The median values for treatment duration ranged from four to nine days, and for daily dosage ranged from 7.30 to 11 mg. Among the participants, 16% (n-13,040) required had no oxygen support requirements within two days of hospitalization, whereas 70% (n=56,368) needed oxygen supplementation.
Further, 9.0% (n=7,618) needed non-invasive positive pressure ventilatory support (NIPPV), whereas 5.0% (n=3,673) needed extracorporeal membrane oxygenation (ECMO) or mechanical ventilatory support (MV). Early dexamethasone use lowered the study outcome for individuals with oxygen supplementation and MV or ECMO requirements, with aOR values of 0.9 and 0.8, respectively.
On the contrary, any cause of within-hospital deaths or discharge for hospice care did not decrease for individuals receiving dexamethasone without any oxygen supplementation and/or NIPPV, with aOR values of 0.9 and 0.9, respectively. Of note, dexamethasone conferred more benefits to individuals with comorbid conditions.
Among individuals receiving oxygen support, the primary study outcome improved among individuals aged above 70.0 years, Whites, non-Hispanics, diabetics, remdesivir non-recipients, individuals with greater CCI scores (aOR 0.9), and individuals who received low-flow oxygen supplementation. Among individuals with NIPPV requirements, the primary study outcome improved among Whites and individuals with greater CCI scores.
Among individuals needing ECMO or MV, the primary study outcome improved among younger individuals, non-Hispanics, and remdesivir recipients. In addition, the sensitivity analysis, performed by limiting outcomes by time epoch (before versus after 1 January 2021), yielded similar results as the primary analysis, indicating that the study findings were robust.
Conclusions
Overall, the study findings showed that among COVID-19 inpatients, administering dexamethasone within 48 hours of hospitalization or supplemental oxygen escalation significantly lowered the probability of COVID-19-associated death or discharge for hospice care among individuals receiving supplemental oxygen, ECMO, or MV.
The observations were directionally consistent, irrespective of supplemental oxygen requirements; however, there was no benefit of systemically administered dexamethasone therapy among those who did not require oxygen supplementation or NIPPV. The study findings underpin the continual usage of dexamethasone among hospitalized COVID-19 patients, especially among elderly individuals with multiple comorbidities.

